Could New Discoveries Revolutionize Treatments for Juvenile Dermatomyositis?
Published: 2025-09-12 02:54:00 | Category: Uncategorized
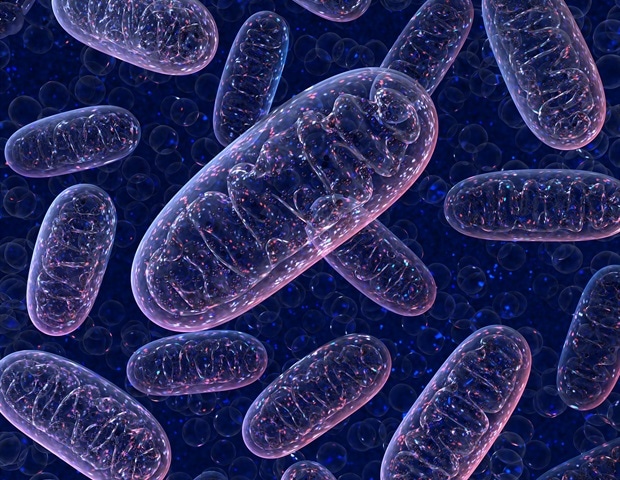
This article explores groundbreaking research on juvenile dermatomyositis (JDM), a rare muscle disease affecting children, which highlights mitochondrial dysfunction as a potential target for future treatments. Conducted by experts at University College London (UCL) and Great Ormond Street Hospital (GOSH), the study offers hope for better therapeutic strategies, especially for those who do not respond well to existing treatments.
Last updated: 05 October 2023 (BST)
Key Takeaways
- Juvenile dermatomyositis (JDM) is a rare disease causing muscle weakness and skin rashes in children.
- New research identifies mitochondrial dysfunction and immune system overactivity as key factors in JDM.
- Current treatments focus on inflammation; future therapies may address mitochondrial health.
- The study was conducted by UCL and GOSH, utilising advanced technology to analyse muscle samples.
- Patient involvement was integral to the research process.
Understanding Juvenile Dermatomyositis
Juvenile dermatomyositis (JDM) is an inflammatory disease that primarily affects children, characterised by muscle weakness and distinctive skin rashes. It triggers inflammation in the capillaries, which are tiny blood vessels, leading to rashes commonly found on the fingers, elbows, and other areas. In severe cases, it can cause calcium deposits in the skin or deeper tissues, restricting joint movement and causing significant discomfort.
JDM has a low incidence rate, with approximately two to four new cases reported per million children each year. However, due to its rarity and the complexities involved in diagnosis and treatment, the actual prevalence of the disease remains challenging to estimate.
Research Insights: Mitochondrial Dysfunction and Immune Response
The recent study published in the Annals of Rheumatic Diseases sheds light on the underlying mechanisms of JDM. Researchers analysed muscle samples from three children diagnosed with the condition and compared them to samples from healthy individuals. By employing a cutting-edge technology known as spatial transcriptomics, the study offered unprecedented insights into gene activity within the muscle tissue.
The findings revealed two critical differences in the muscle samples from JDM patients:
- Mitochondrial Dysfunction: Researchers identified that the mitochondria, which are essential for energy production within cells, were not functioning correctly in the muscle tissues of children with JDM. Remarkably, this dysfunction was present even in muscles that appeared healthy.
- Immune System Activation: The study highlighted an overactive immune response, known as interferon activation, where the immune system mistakenly targets the body's own tissues as if fighting an infection. This response can contribute to feelings of weakness and fatigue in affected children.
While the immune system's role in JDM is well-documented, this research marks the first time that these two problems have been mapped in detail within muscle tissue, offering new perspectives on potential therapeutic targets.
Implications for Treatment
The implications of this research are significant, particularly in terms of treatment strategies. Current therapies primarily aim to reduce inflammation through the use of corticosteroids and immunosuppressants. However, the identification of mitochondrial dysfunction as a contributing factor opens the door for novel treatment approaches that focus on improving mitochondrial health.
Professor Lucy Wedderburn, the senior author of the study and a consultant paediatrician at UCL Great Ormond Street Institute of Child Health, emphasised the importance of these findings. She stated, "This research suggests that we should not only focus on calming the immune system but also consider strategies to fix the mitochondria."
Real-life Impact: Lucia's Journey
Five-year-old Lucia from Twickenham, who was diagnosed with JDM in August 2024, embodies the challenges faced by children with this condition. Her symptoms began during a family trip to New Zealand over Christmas 2023, when her parents noticed a red rash on her fingers and toes. Initially attributing it to the cold weather, they grew concerned as the rash persisted and worsened.
Upon returning to the UK, Lucia underwent a series of consultations with specialists, eventually being seen by Dr Clarissa Pilkington at GOSH, who diagnosed her with JDM. Lucia's treatment regimen included corticosteroids and methotrexate, an immunosuppressant. However, due to suboptimal response, her treatment shifted to intravenous immunoglobulin therapy, requiring monthly hospital admissions.
Her father, William Magee, expressed his optimism regarding the recent research findings, noting that they could pave the way for treatments that address the root causes of JDM rather than merely alleviating symptoms. "It’s reassuring to know that this could lead to more effective treatments," he stated.
The Path Forward: Research and Future Directions
Dr Merry Wilkinson, co-lead of the study, underscored the need for continued investigation into mitochondrial health in JDM patients. The research team aims to explore existing medications and develop new treatments that could enhance mitochondrial function while minimising side effects. The study was part of the Juvenile Dermatomyositis Cohort and Biobank project, recognised as one of the largest databases of clinical and biological samples related to JDM globally.
Importantly, patient involvement played a crucial role throughout the research process. Families contributed not only by providing muscle samples but also by participating in discussions about study design and outcomes. This collaboration ensures that the research remains relevant and focused on the real experiences of those living with JDM.
Conclusion: A Hopeful Future for JDM Patients
The findings from this pivotal research represent a significant step forward in understanding juvenile dermatomyositis. By highlighting the dual roles of mitochondrial dysfunction and immune response, the study lays the groundwork for future therapeutic strategies that could improve the quality of life for children affected by this debilitating condition. As researchers continue to explore these avenues, the hope is that treatments will evolve, allowing children like Lucia to spend less time in hospital and more time engaging in everyday activities.
As we look towards the future, one can only wonder how these advancements in understanding JDM will shape the landscape of paediatric medicine. What other hidden mechanisms might research uncover in rare diseases, and how might these insights transform lives? #JuvenileDermatomyositis #MitochondrialHealth #ChildrensHealth
FAQs
What is juvenile dermatomyositis?
Juvenile dermatomyositis (JDM) is a rare autoimmune disease that affects children, causing muscle weakness and distinctive skin rashes due to inflammation in blood vessels.
How common is JDM?
JDM occurs in approximately two to four new cases per million children each year, making it a rare condition. However, its actual prevalence is difficult to estimate.
What are the main symptoms of JDM?
Symptoms of JDM include muscle weakness, skin rashes, calcium deposits under the skin, and potential complications affecting other organs such as the lungs and intestines.
What treatments are currently available for JDM?
Current treatments for JDM primarily focus on reducing inflammation using corticosteroids and immunosuppressants. New research suggests that addressing mitochondrial dysfunction may lead to more effective therapies.
How can parents get involved in research for JDM?
Parents can support research by participating in clinical studies, contributing samples, and engaging with researchers to share their experiences and insights regarding JDM.



